COVID-19 & Biological Inequality; a London Data Study
May 2020
-
Therefore, this paper investigates how COVID-19 is interacting with urban environments that are high in systemic deprivation and environmental stressors and their communities, specifically Black, Asian and minority ethnic (BAME) communities in the UK.
The current discussion is focusing on systemic racism and inequality, which is correct. However, this focus can easily be seen as not relevant to those that are planning or designing environments, as they might not qualify it as their domain. Therefore, this paper will look to approach it from a biological perspective, drawing a clear throughline between human health and urban environments. Specifically, this paper will look at the phenomenon of biological inequality and its relation to COVID-19 in BAME communities of London.
-
A person can only have agency over their health when they are part of a supportive ecosystem, which includes the places they inhabit.
It is not a matter of being BAME that is a health risk, it is the conditions and environments BAME communities are forced to engage with that is the health risk. In other words BAME communities are more at risk due to the environments they are forced to live in due to racism and inequality.
Although no causal relationships can be inferred, we can tentatively propose that deprivation and structural racism may be a cause for the high number of deaths by COVID-19 among BAME communities, who are often living in poorer environments

it is not a matter of being BAME that is a health risk, it is the conditions and environments BAME communities are forced to engage with that is the health risk. In other words BAME communities are more at risk due to the environments they are forced to live in due to racism and inequality.
Abstract
It is now well understood that poorly designed and planned environments heighten the risk of health issues due to systemic deprivations and stressors. Therefore, this paper investigates how COVID-19 is interacting with these environments and their communities, specifically Black, Asian and minority ethnic (BAME) communities in the UK. As COVID-19 continues to spread through the British population a trend has emerged, poorer ethnic minority communities are the ones being most affected, both in hospitalisations and death rates. According to the most up to date Office for National Statistics (ONS) Black people are almost twice as likely to die from COVID-19 than white counterparts, additionally, Bangladesh/Pakistani people are ~1.7 times more likely to die than white counterparts.
The current discussion is focusing on systemic racism and inequality, which is correct. However, this focus can easily be seen as not relevant to those that are planning or designing environments, as they might not qualify it as their domain. Therefore, this paper will look to approach it from a biological perspective, drawing a clear throughline between human health and urban environments. Specifically, this paper will look at the phenomenon of biological inequality and its relation to COVID-19 in BAME communities of London.
Introduction
When investigating the effects of poverty in the context of Western countries, it is important to identify two elements. The first is to identify “who” is experiencing poverty and the second is identify “where” poverty is taking place. Through the systemic application of racism, studies in the US have shown that it is predominantly ethnic minorities that are forced to live in poorly planned environments. The parameters of a poorly planned environment are defined in this paper as places with high levels of environmental pollutants (air, noise, light, thermal), inadequate housing infrastructure, inadequate access to blue and green infrastructure, low access to nourishing food, inadequate urban infrastructure, poor access to public transport, and poor access to adequate health resources. These environments have been the source of hundreds of epidemiological studies, yielding a well substantiated theory, which identifies poverty as a health risk. For instance, people living in low income households in the UK are two to three times more likely to develop mental health problems.
In order to advance policies that put health at their core, poverty must be addressed and understood beyond the confines of economic statistics. Poverty is supported by racism, executed through urban systems, and experienced through poor health. A significant example of how racism, poverty, and health interact was shown in a study of diabetes conducted in the East Side of Manhattan (NYC). From East 96th Street upwards (East Harlem) diabetes took a more lethal and detrimental turn; in these neighbourhoods the disease caused more amputations, blindness, and death. In contrast from East 96th street downwards (Upper East Side), diabetes was not life threatening or as severe. The main differentiator was poverty: East Harlem’s poverty rate is 31.5% in comparison to the Upper East Side 6.1%. Furthermore, East Harlem is a predominant Latinx and African-American area, whereas the Upper East Side is predominantly White. This culmination of events is what is termed as structural racism, which is defined as macro level systems such as social forces, institutions, ideologies, and policies, that interact with one another to generate and reinforce inequities among specific ethnic groups.
Whilst the bulk of the literature on health inequalities has mainly focused on the US, the UK is also experiencing similar challenges. For instance, in England, black and Pakistani people are more likely to live in the 10% of neighbourhoods most deprived in relation to living environment (16% and 27% respectively did so). Additionally, Pakistani and Bangladeshi people were over 3 times more likely than White British people to live in the most deprived 10% of neighbourhoods in England.
Now that the world is facing a pandemic, which has shown to disproportionately affect BAME communities. It is important to have a deeper biological understanding of these health disparities caused by the intersection of poverty, racism, and poor urban planning. The contribution of this paper is on the biological parameters of this phenomena, specifically the stress response and allostatic load, which play a key role in disease pathology.
This study will look at mapping where BAME communities live and its relation to COVID-19 rates.
Relevance Of This Study
The backbone of this study is how biology interacts and is affected by the built environment. This line of study was selected for two reasons, the first is to illustrate that poor urban planning puts a burden on an individual’s stress response increasing the risk of disease. Secondly, understanding how the built environment creates a health risk can lead to better urban planning strategies and policies. One of the first studies linking health to impoverished environments was a 1939 study on Schizophrenia in Chicago. This is a clear indication that it is time for change by applying strategic changes to urban planning.
COVID-19 has highlighted the health emergency sweeping our cities, which need to be critically addressed. It is evident that without health, human progress is stalled.
Stress Response, Impoverished Urban Environments & Disease
To gain further insight into the higher death rates of COVID-19 amongst BAME communities, a biological framework has to be established. This paper, proposes a framework using two significant factors; the physical environments people inhabit and the experiences afforded by those environments. There are three reasons these factors are important, the first is they can be linked to the human biological system via the stress response, secondly, these elements are highly influenced by systemic racism. Thirdly, understanding the role neighbourhoods play in health allows for health to be solved at a systemic level.
A person can only have agency over their health when they are part of a supportive ecosystem, which includes the places they inhabit.
To recognise how the places people inhabit and their experiences shape, influence, and interact with human biology an understanding of the stress response is necessary. The stress response is the main pathway linking the world around us with our health as it is a fundamental biological mechanism through which our bodies adapt to changing conditions (stimuli) in the environment that threaten biological stability, known as stressors. People encounter a variety of stressors categorised in two overarching types; internal and external. An example of an internal stressor could be responding to a change within the body, such as a virus. External stressors have two further distinctions, environmental and psychological. Environmental stressors are related to the physical environment, they can include air, noise, light, or thermal pollutants. In terms of psychological stressors, these relate to experiences, such as starting a new job or losing a loved one.
The stress response is mitigated by the hypothalamic-pituitary-adrenal axis (HPA-Axis). In simple terms, its activation begins when a stressor triggers the hypothalamus, which is located in the brain to produce and release the corticotropin hormone (CRH). This trigger then signals the pituitary gland, also located in the brain, to synthesise the adrenal-corticotropin releasing hormone (ACTH). ACTH is then released into the circulation system where it reaches the adrenal glands, which are located above the kidneys. Once it reaches the adrenal glands ACTH stimulates the release of cortisol, another regulatory hormone. Finally, cortisol circulates back to the brain through the circulatory system. Current understanding is that this cycle of hormones repeats in a negative feedback loop until the body reaches stability. This is called allostasis, a process by which “an organism maintains physiological stability by changing the parameters of its internal milieu, matching them appropriately to environmental demands”.
The adaptation to stressors requires the HPA-Axis to interact with various other major systems such as endocrine, immune and metabolic. This interaction with the environment is long standing and it's fundamental to how any biological system navigates and interacts with all aspects of their environment. However, when the stress response is chronically engaged, due to persistent exposure to stressors it may prevent the body from reaching allostasis, leading to what is called allostatic load (AL). Allostatic load is known as the “wear and tear” of bodily systems, which overtime can impair the function of the immune response. Herein lies one of the biomarkers in the pathology of a wide range of diseases, specifically metabolic disease (diabetes, obesity, cardiovascular) as well as mental disorders (PTSD, depression, and anxiety).
In order to fully understand the biological mechanisms behind the disproportionate number of deaths in the BAME communities in London, AL needs to be contextualised to where BAME communities live and their experiences generated through those environments. As it has already been mentioned BAME demographics disproportionately experience higher levels of poverty. Additionally, poor ethnic minorities disproportionately live in areas with higher levels of air, noise, and light pollution, lower levels of green spaces, and higher exposure to urban heat island effect. All of these can be classified as stressors, taking air pollution as an example, the stress response engages at first contact, triggering one of the earliest biological responses to the pollutant. The response will continue until exposure has ended, therefore, the longer a person lives in these environments, the longer the stress response will engage, risking AL.
Housing should be considered as another physical environment where poverty is experienced, as the housing quality of these demographics is another source of stressors. Poverty often means living in inadequate homes that have poor ventilation, overcrowded spaces, and poor basic infrastructure (no running water, poor heating/cooling). In turn, these conditions require the stress response to engage. For example, overcrowding has become a topic of interest as it is a contagion facilitating factor contributing directly to COVID-19. However, it is not just a question of contagion, overcrowding also has two stress pathways, which can contribute to poor health. The first is through noise pollution: overcrowded spaces are often noisier due to human activity happening in close proximity. Noise pollution can cause the stress response to engage as it can change the body's blood pressure. The second pathway is the psychological experience of overcrowding, which can also be stressful through a multitude of scenarios: perceiving a lack of privacy, lack of personal personal space, lack of psychological safety or lack of restorative space.
The second factor in the biological framing are the experiences lived in these types of environments. In terms of poverty, they are specifically classified as psychosocial stressors, which refer to a person having external demands that exceed their perceived abilities and resources to adequately respond to a specific event. For instance, a psychosocial stressor would be triggered by lack of appropriate financial resources while still having to provide for rent, food, or childcare. It can also refer to the awareness of not having enough heat to warm up the household or not having the comfort of secure long-term shelter. Psychosocial stressors are well known to have biological correlates of AL.
Whilst the experience of stress is a natural part of biological existence, living in impoverished environments exposes people to persistent stressors, risking AL, which in consequence can heighten the risk of disease.
Disease Susceptibility and COVID-19
The persistent and disproportionate exposure to environmental and psychosocial stressors has been identified and defined by the Centric Lab as biological inequality. Biological inequality puts a burden on the stress response contributing to its dysregulation (AL). Over time, this dysregulation impacts immune, metabolic, and endocrine systems, making people more susceptible to a wide range of diseases.
Susceptibility in this paper refers to the heightened risk of developing diseases and suffering more acute symptomatology compared to a normative population, due to being disproportionately experiencing biological inequality. There are two pathways between COVID-19 and susceptibility. The first is BAME communities due to biological inequality are more susceptible to diabetes, asthma, depression, and obesity, which have been identified as risk factors for COVID-19. These types of disorders cause inflammation in the body due to dysregulation of the immune system, which in turn is linked to allostatic load. In turn these biological changes can heighten the risk of viral contraction, severity of symptoms, and death in relation to COVID-19.
The second pathway is directly through allostatic load, which means that a person may not seemingly have an underlying disorder, however, due to living in biological inequality, their stress response is more likely to be significantly dysregulated. In a study on respiratory infections, the “rates increased in a dose-response manner with increases in the degree of psychological stress”. This mechanism could in part explain the reason Black communities were still twice more likely to die of COVID-19 even when adjusting for health (i.e. comorbidities). This would require further medical study to look at AL levels in BAME communities as well as other health inequalities that are yet to be understood.
Two caveats should be highlighted, the first is susceptibility is not the same as determinism. In other words, being susceptible to disease does not mean that a person will certainly develop a disease as there are many other factors which contribute to disease pathology. For example, a study conducted in the US, indicated that having emotional support can offset some of the effects of neuroendocrine, metabolic, inflammatory, profiles that tend to develop after exposure to acute and persistent stress.
There is a second caveat, it is not a matter of being BAME that is a health risk, it is the conditions and environments BAME communities are forced to engage with that is the health risk. In other words BAME communities are more at risk due to the environments they are forced to live in due to racism and inequality.
Materials, Methods, Results, and Discussion
In order to map the susceptibility and COVID-19 within BAME communities the study collected four data sets. Index of Multiple Deprivation, Stress Risk Score, Areas of Health Risk, and Office of National Statistics.
The Index of Multiple Deprivation (IMD) is the official measure of relative deprivation in England and is part of a suite of outputs that form the Indices of Deprivation (IoD). It follows an established methodological framework in broadly defining deprivation to encompass a wide range of an individual’s living conditions.
Income. (22.5%)
Employment. (22.5%)
Education. (13.5%)
Health. (13.5%)
Crime. (9.3%)
Barriers to Housing and Services. (9.3%)
Living Environment. (9.3%)
People may be considered to be living in poverty if they lack the financial resources to meet their needs, whereas people can be regarded as deprived if they lack any kind of resources, not just income. Due to the robustness of the IMD it was used as a proxy for psychosocial stressors related to living in areas of deprivation.
The Stress Risk Score (SRS) is a scale used to measure the environmental stress risk factors based on proxies for noise, air, light, and thermal pollution, this has been done using a meta-analysis of how each stressor engages with the stress response, specifically allostatic load. The SRS is based on a linear scale of 0 to 4, with 0 being a less polluted area and 4 being highly polluted across four environmental stressors. The total score is obtained by summing the means of the individual pollutant scores. These individual scores are divided into bins from 0 to 1 based on thresholds from past neuroscientific research on pollutant effects on health that are mediated through stress-related pathways. The thresholds are maximum values that the pollutant can reach before human health is significantly at risk. The SRS was used to look at environmental stressors
Areas of Health Risk (AHR) is a calculation based on combining IMD and SRS to determine where there is a susceptibility to disease based on exposure to environmental and psychosocial stressors.
The Office of National Statistics (ONS) database was referred to when obtaining data on: age-standardised mortality rates for all causes and deaths involving COVID-19, local authorities in England and Wales, deaths per 100k occurring between 1 March and 17 April 2020, and the 2011 England and Wales Census on BAME population density per 100k.
Methods
The IMD, SRS, and AHR scores were averaged at the borough-level. A Pearson’s correlation between COVID-19 positive cases and each of the IMD 2019. The study uses these data points to map Structural Racism (this highlights that BAME communities disproportionately live in areas of high IMD) (figure 1).
Results
Correlate Results
The data indicates high correlation between COVID-19 deaths and IMD 2019 by borough (r = 0.73), between COVID-19 deaths and BAME population density (r = 0.83), and between IMD 2019 and BAME population density (r = 0.62) (see Table 1). Moreover, a medium-low correlation was also observed between SRS and BAME density and SRS and COVID-19 deaths (r = 0.21 and r = 0.23 respectively).
| R VALUE | Domain 1 Correlation | Domain 2 Correlation |
|---|---|---|
| 0.73 | IMD 2019 | COVID-19 deaths per 100k people |
| 0.83 | BAME density per 100k population | COVID-19 deaths per 100k people |
| 0.62 | BAME density per 100k population | IMD 2019 |
| 0.41 | SRS | IMD 2019 |
| 0.21 | SRS | BAME density per 100k population | 0.23 | SRS | COVID-19 deaths per 100k people |
Table 1. Summary of correlation values between COVID-19 deaths, BAME population density, SRS and IMD in London using Pearson correlation.
Discussion
The high correlations indicate a strong positive relationship between deprivation and death by COVID-19, as well as highlighting a possible trend of increased number of deaths among BAME communities. Secondly, in terms of biological inequality, environmental stressors (SRS) whilst a positive correlation (r=0.21) is not as high when compared to psychosocial stressors (IMD) which is at a very high correlation (r=0.73). This could indicate that psychosocial stressors could play a more significant role in AL than environmental stressors, it could also indicate that psychosocial stressors are more prevalent and persistent than environmental stressors.
Composite Results
Figure 1. Structural racism in London (deprivation): BAME population density (per 100k population) overlapped with deprivation (IMD decile 2019). The darker purple colours are the areas where high BAME population density intersects with high deprivation. The London Borough of Newham scores the highest.
Figure 3. Structural racism (all domains). BAME population density (per 100k population) overlapped with pollution (SRS scores) and deprivation (IMD decile 2019), where darker red = highest structural racism. The London Borough of Newham again scores the highest.
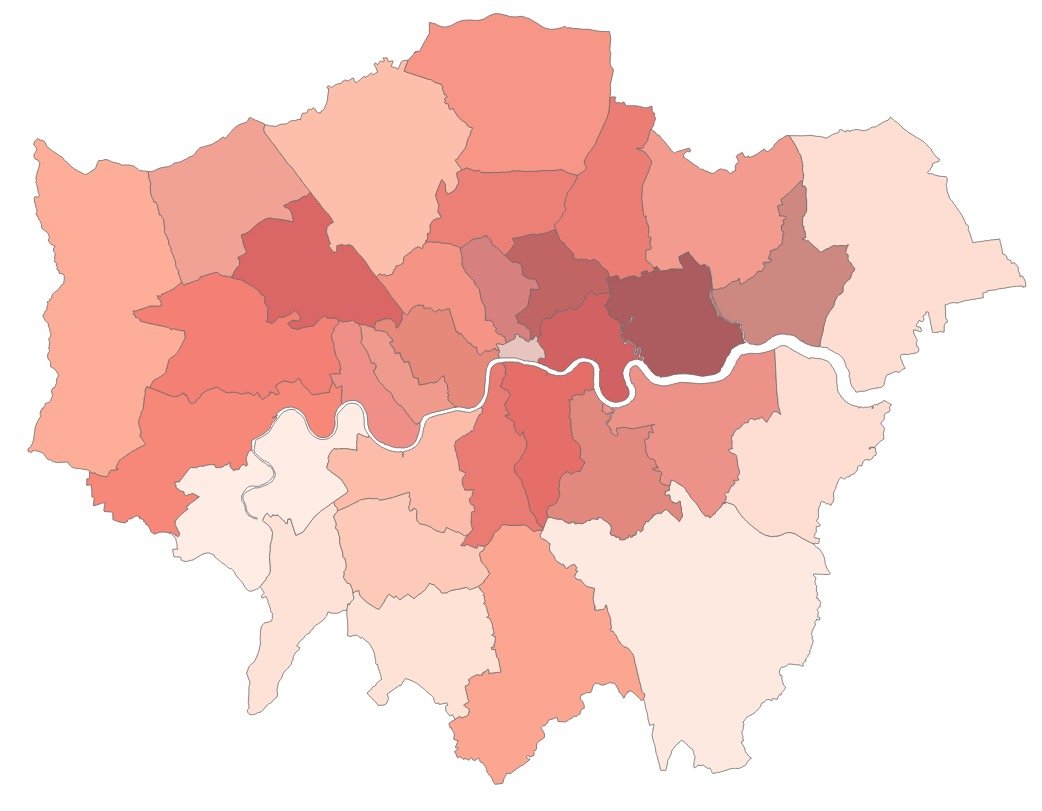
Figure 5. COVID-19 deaths as of 17/04/2020 (darker red = more deaths per 100k population). Newham and Brent are the most affected areas, followed by Hackney and Tower Hamlets.
Figure 6. Structural racism (all domains). BAME population density (per 100k population) overlapped with pollution (SRS scores) and deprivation (IMD decile 2019), where darker red = highest structural racism. Newham again scores the highest.
Figure 2. Structural racism in London (pollution): BAME population density (per 100k population) overlapped with pollution (SRS score). The darker purple colours are the areas where high BAME population density intersects with high pollution. The London Borough of Newham scores the highest.
Figure 4. Areas of health susceptibility due to biological inequality (Inclusive of all ethnic demographics). Deprivation (IMD decile 2019) was overlapped with SRS scores, showing areas of high pollution and deprivation, posing a risk to health (darker purple = higher risk). Hackney scoring the worst followed by Tower Hamlets, Southwark, Camden, Westminster, and Kensington & Chelsea.
Biological Inequality and COVID-19 death rates: Inclusive of all ethnicities.
Figure 7. COVID-19 deaths as of 17/04/2020 (darker red = more deaths per 100k population). Newham and Brent are the most affected areas, followed by Hackney and Tower Hamlets.
Discussion
Although no causal relationships can be inferred, we can tentatively propose that deprivation and structural racism may be a cause for the high number of deaths by COVID-19 among BAME communities, who are often living in poorer environments. Figures 1, 2, 3 below show various aspects of structural racism in London, by overlapping data on deprivation and pollution to BAME population density. This is an important factor to note as it highlights that BAME communities are more likely to be zoned in areas that have psychosocial stressors (IMD) and environmental stressors (SRS). Therefore biological inequality which is the composite of IMD and SRS is disproportionately experienced by BAME communities in London.
In terms of COVID-19 when the death rate map was compared to the composite map of health risks due biological inequality map (figure 4) there is a strong overlap. For example, Hackney and Tower Hamlets have both high COVID-19 death rates and high health risk. This is an indication that identifying hotspots prior to the pandemic could have been useful to deploy extra resources for those areas. The maps also indicate that susceptibility though a strong factor in disease pathology is not deterministic as other factors such as jobs, emotional support through social cohesion, diet, and other health indicators are also at play. Conversely, in the composite map of BAME population, IMD, and SRS is compared to the COVID-19 (figure 6) death rate map (figure. 7) there is an even stronger overlap, indicating that BAME communities could be experiencing unique health inequalities than the general population. Some possible scenarios are that BAME communities could be living in these areas for longer, the jobs they hold could also be exposing them to further stressors, or they have less access to health facilities. This is worth further investigation at a population level.
Finally, even though it is not causal, structural racism plays a role in the story of COVID-19. It manifests in BAME communities being zoned to areas of higher environmental pollutants and deprivation. This in turn has made these communities more susceptible to chronic disorders which have heightened both the risk of contracting COVID-19 as well as experiencing higher death rates.
Limitations
The limitations with any borough level analysis is the direct relation to individual lifestyles and risk factors as some factors are too nuanced to be analysed at such a large scale. The way to overcome this limitation is by ecological research and interventions that incorporate more personal information and demographics, and individual risky or compromising behaviour such as commute, exercise, travel, or smoking.

Further Investigations & Actions
It is important to note that this is a preliminary analysis of COVID-19 and how it relates to biological inequality brought on by systemic racism. Secondly, as this is a preliminary study due to pending datasets as the pandemic is on-going it does highlight the following future needs, investigations, and actions.
Future Investigations.
A deeper study in variations of environmental stressors and COVID-19 cases, especially those living in areas that have higher levels of air and thermal pollution. This is relevant to understand how an increase in car traffic during summer months plays a role in respiratory recovery and health.
Do a final study with the full death rates after the second wave.
Look into specific social demographics such as children, elderly, men, and women.
Longitudinal epidemiological study to look at the long term secondary effects of COVID-19 in these areas. The secondary effects being trauma due to experiencing death and illness of direct members of their community. Especially in relation to how children in these hotspots will be affected as they age.
Future Actions
Better lexicon and frameworks to discuss health. Health is not merely the absence of disease, health is the ability for our biological systems to enter stability after experiencing trauma or stress throughout our entire lifetime, to give us all an equal opportunity to realise our full potential.
The COVID-19 pandemic has highlighted the fragility of the healthcare system in many Western countries and has shed light on the differences in health accessibility and susceptibility of various communities in large cities. We have a chance to further the narrative on how we must approach community health to make our cities more resilient. The unexpected rise and spread in cases, as well as the high mortality rates compared to Asia-Pacific countries, questions the preparedness of Western countries to tackle health emergencies - which are bound to increase with future natural disasters due to climate change. We have hereby shown that a positive relationship between COVID-19 spread and levels of deprivation and pollution can be drawn in London, the worst-hit area of the UK. We predict that, as the pandemic develops, the correlation between the three will increase further, reflecting areas of health emergencies. We urge governments and local councils to direct resources for improving health risk areas in the near future. These authorities must also acknowledge that workers and members of the community who cannot afford to self-isolate due to their contributions to the community are a susceptible population and address this in any future community health infrastructure.
The COVID-19 pandemic should serve as a lesson on how to prevent and contain future health emergencies, which are likely to become more frequent as climate change poses an impending threat. We can already analyse that pandemics/epidemics will likely take place at the same time as natural disasters, which will hinder efforts to contain the spread of diseases because of people being displaced. Lack of adequate housing, epidemics, and natural disasters pose large threats to the future of human health and life and need to be addressed immediately.
Finally, this information can be useful to mobilise change from the bottom up through community activism. Citizens can now ask local governments for better housing and urban realm design, especially as these communities will need to prepare for a second wave of COVID-19.
For policy and Urban Planners & designers of the urban realm it is important that responsibility is taken to improve areas of biological inequality as they make people susceptible to disease. This is especially relevant as many councils and planning authorities move towards health based drivers and metrics. This paper has shown what happens when environments are poorly planned, furthermore it shows that London is not a city that has health resilience and thus vulnerable to the effects of crisis, either through a pandemic or climate change.
For further inquiry and investigation please contact Araceli Camargo.